-
![Dried flowers in a glass jar casting a shadow on the wall.]()
Recurrent thrush
“Why does thrush keep coming back?”
This is something I hear from so many women.
You treat it with creams or tablets, it clears up for a while… and then it’s back again. Frustrating, right?
Recurrent thrush is rarely just about the yeast itself.
It’s usually a sign that something deeper is out of balance — most often in:
• the gut microbiome
• the immune system
• or hormonesThat’s why local treatments only give temporary relief.
In my practice, I take a step back and look at the bigger picture:
1. Nutrition first. Yeast thrives on sugar and refined carbs. Cutting these down and swapping in more whole foods, berries, and nuts can make a huge difference.
2. Gut support. Around 80% of your immune system is linked to the gut. More fiber and fermented foods help create natural protection.
3. Lifestyle shifts. Lack of sleep and chronic stress lower immunity and make thrush more likely to return. Rest and stress management are part of the healing process too.
✨ For many women, these changes are enough to finally stop the cycle.
But if the problem continues, that’s when I bring in functional testing.
These tests can reveal hidden triggers — like nutrient deficiencies, microbiome imbalances, or hormonal issues — that we wouldn’t see otherwise.
Once we identify the real root cause, treatment becomes much more effective.
If you’ve been struggling with recurrent thrush, please know: you don’t have to just put up with it. With the right approach, there is a way out of the cycle.
Send me a message if you’d like to find out where to start.
-
![Two black coffee cups on matching saucers placed on a round wooden table.]()
Is Your Brain in a Sleep Debt Spiral?
Why do we feel sleepy in the evening? It all comes down to adenosine—a molecule that builds up in our brain throughout the day. The longer we stay awake, the more adenosine accumulates, making us feel increasingly tired.
When we sleep, our brain works to clear out adenosine so that we wake up refreshed. But here’s the catch: if you don’t sleep enough, adenosine isn’t fully cleared. You wake up with an already elevated level, meaning your brain is still in “sleep debt” from the day before. And just like financial debt, it keeps accumulating if left unpaid—leading to chronic fatigue, poor focus, and reduced performance.
Now, what about caffeine? Many people assume it “gives energy,” but in reality, it only blocks adenosine receptors, preventing your brain from recognizing how tired you truly are. The adenosine is still there, silently stacking up. And once your liver metabolizes caffeine, the full weight of your accumulated fatigue crashes down on you.
Here’s where genetics come into play: the CYP450 enzyme in your liver determines how quickly you process caffeine. Some people break it down rapidly, while others metabolize it slowly—meaning even a morning coffee can interfere with sleep at night.
If you wake up tired, even after 6-7 hours of sleep, or struggle to fall asleep at night, your body might be trapped in this adenosine accumulation cycle.
In my practice as a functional medicine doctor, I focus on lifestyle medicine—optimizing factors like sleep, caffeine intake, and energy regulation to help people break free from chronic fatigue. -
![New Normal?]()
What’s “common” isn’t always “normal.”
As a functional medicine doctor, I often hear patients say things like, “I’ve always been like this” or “That’s just normal for me.” But just because something has been happening for years doesn’t mean it’s healthy or optimal for your body.
For example, infrequent bowel movements—perhaps only once every 4-5 days—might feel “normal” because you’ve adapted to it. But in reality, this isn’t normal and could be a sign of underlying imbalances that deserve attention.
The challenge? Many people don’t mention these symptoms to their doctor because they don’t think they’re relevant or problematic. But those seemingly small, overlooked patterns can often be the key to unlocking deeper health insights.
This is why I encourage everyone to take a step back and critically review their symptoms. Don’t dismiss something just because it’s been happening for a long time. Listen to your body, and don’t hesitate to bring up what you might consider “minor” issues with your healthcare provider—they’re often more important than you realize.
Your health is worth investigating. Let’s redefine what’s truly “normal.” -
![Blurred image of flower and leaves behind a frosted glass or plastic surface.]()
Brain fog
Have you ever experienced brain fog? That feeling of mental cloudiness, where focus, memory, and clarity seem just out of reach?
Brain fog isn’t a diagnosis, but a symptom with multiple possible causes. It can be triggered by:
• Chronic stress
• Poor sleep quality
• Nutritional imbalances
• Hormonal fluctuations (like thyroid issues)
• Food sensitivities
• Chronic inflammation or infections
What makes brain fog complex is that the root cause varies from person to person. One person’s fog might stem from stress and lack of sleep, while another’s might be due to a nutrient deficiency or underlying health condition.
Because the causes are diverse, the treatment has to be highly individualized. There isn’t a one-size-fits-all approach. A tailored strategy that looks at your unique lifestyle, diet, and health status is essential for addressing the root cause, not just managing the symptoms.
In functional medicine, we take a holistic approach to uncover these underlying factors and create personalized treatment plans.
If you or someone you know is experiencing brain fog, it’s worth exploring the deeper, underlying issues. It’s time to clear the fog by addressing the root cause, not just the symptoms. -
![]()
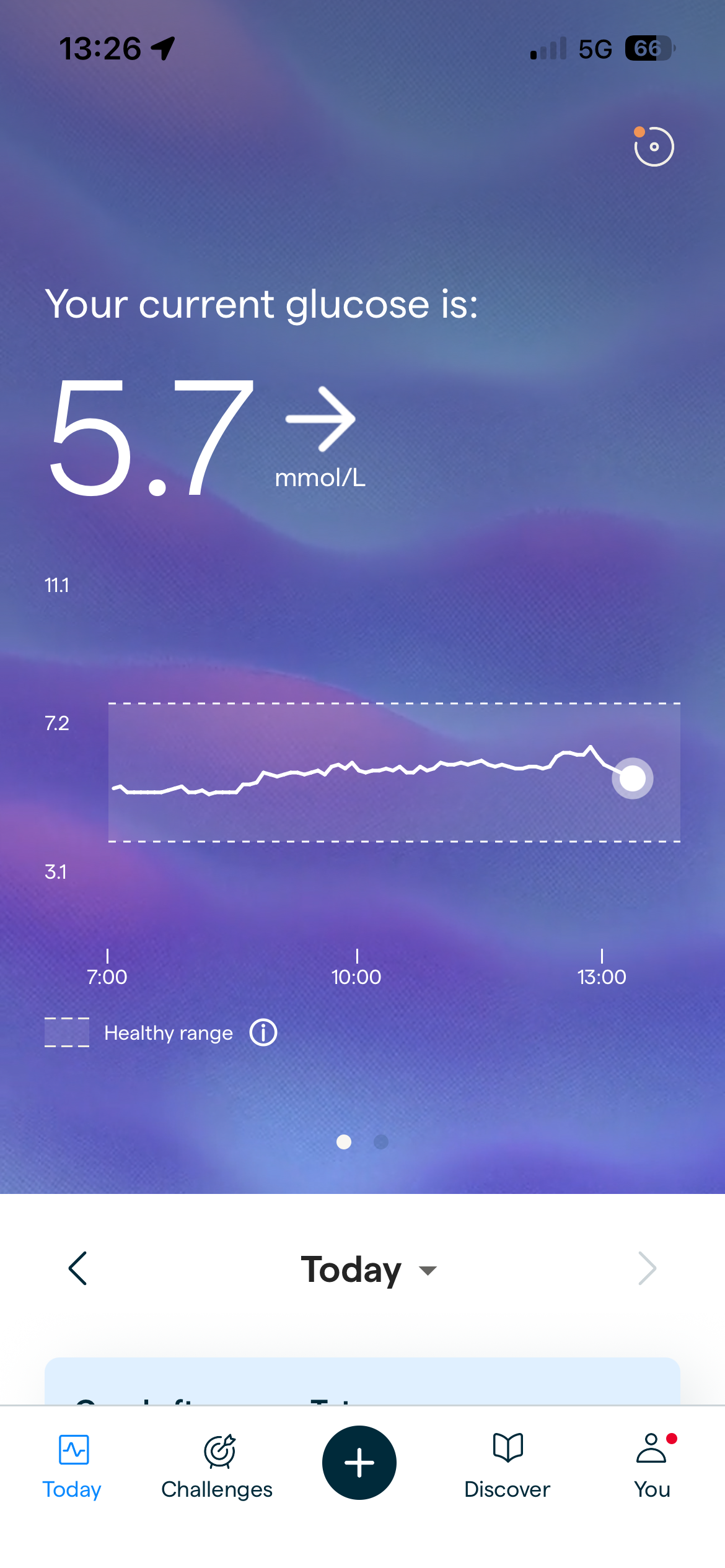
BLOOD SUGAR AND MENTAL CLARITY
Blood sugar plays a much bigger role in daily well-being than most people realise.
Your energy levels, mental clarity, ability to focus, and even mood are closely tied to glucose. It is the primary fuel for the brain, muscles, and many other cells in the body.
The body works continuously to keep blood sugar within a narrow, optimal range. This balance is essential for stable performance and long-term health.
When glucose runs too high, it stops being helpful and starts causing damage. Blood vessels, nerves, and tissues are affected over time. When glucose drops too low, the brain is the first to feel it. Fatigue, brain fog, shakiness, and anxiety can appear quickly.
To prevent these extremes, the body relies on a tightly regulated system known as glucose homeostasis. This process runs in the background at all times, whether you are eating, sleeping, or working.
One way to understand it is to think in financial terms. Blood glucose is like money in a checking account. It needs to be readily available, but not overflowing and not completely depleted.
The liver acts as the central regulator in this system. After meals, when glucose levels rise, some of that energy is used immediately by cells. The excess is sent to the liver, where it is stored as glycogen.
Glycogen is a short-term energy reserve. It allows the body to stay stable between meals and overnight.
When you have not eaten for several hours or while you are asleep, the liver releases glucose from glycogen back into the bloodstream. This keeps blood sugar steady and ensures a constant energy supply for the brain and other vital organs.
When this system functions well, you barely notice it. Energy feels consistent, cravings are manageable, and concentration is easier to maintain.
In the next posts, I will explore what disrupts this balance, why it happens, and why addressing it matters for both metabolic health and everyday performance.Activate to view larger image,